What does Glutathione have to do with Parkinson’s Disease?
What is Parkinson’s Disease?
Parkinson’s Disease affects approximately 10 million people worldwide, and is ranked as the 14th most common cause of death in the United States. This neurodegenerative disorder affects primarily dopamine-producing neurons in a specific area of the brain called substantia nigra.
Symptoms typically develop slowly and often included tremors, bradykinesia, limb rigidity, and gait and balance problems. While there is no cure, treatment options are available (1).
What is Glutathione?
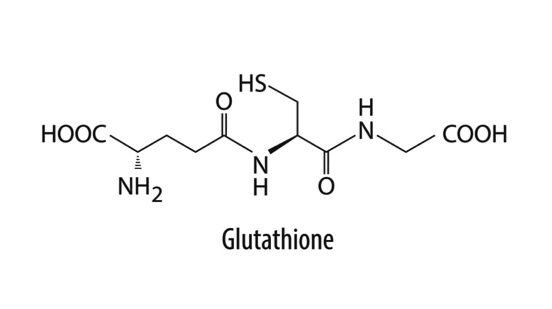
Glutathione is a multifunctional tripeptide, composed of three amino acids including cysteine, glutamic acid, and glycine. It acts as an antioxidant and a cofactor for the enzyme glutathione peroxidase (2, 3).
Why is Glutathione beneficial in patients with Parkinson’s Disease?
“Glutathione is depleted early in the course of Parkinson’s Disease, and deficiency has been shown to perpetuate oxidative stress, mitochondrial dysfunction, impaired autophagy, and cell death,” (4). Therefore, it has been suggested to replete glutathione as a therapeutic intervention. One particular study investigated intranasal administration of glutathione and found it to increase glutathione levels in the brain (4).
Glutathione is known to play an important role in our mitochondria. If glutathione levels are depleted, our mitochondria may become dysfunctional. In fact, the reverse is also true. Mitochondrial stress and dysfunction are known to deplete glutathione levels (5). However, when there is mitochondrial dysfunction, coenzyme Q10 (CoQ10) can be used to restore normality. To this point, research has shown a statistically significant reduced rate of the disease progression after the administration of CoQ10 among patients with Parkinson’s Disease (4).
Additional Benefits of Glutathione
- May support healthy liver function by removing harmful substances
- May enhance immune response, improve immune cell health, and promote the body’s ability to fight disease
- Inhibits the activity of tyrosinase and production of melanin to prevention skin pigmentation
Recommendations to Raise Glutathione Levels (6)
- A typical recommended dose of oral glutathione is > 50 mg/day.
- Cysteine or antioxidant supplementation may raise glutathione levels in the body.
- Vitamin C plays a similar role to glutathione which suggests a sacrificial role to prevent glutathione from being used.
- Lipoic acid appears to raise glutathione levels as well.
- Other supplements that might raise glutathione levels include N-acetylcysteine, glutamine, methionine, and S-adenosyl methionine (7).
Recommendations for Patients with Parkinson’s Disease (8)
- Aside from increasing glutathione levels, try optimizing your diet by avoiding or reducing alcohol and caffeine which may reduce the toxic load on your body’s detoxification pathways.
- Reduce homocysteine to a healthy level by including folic acid, vitamin B12 and B6, zinc, and trimethyl-glycine. Some of these nutrients are cofactors for dopamine production
- Increase omega-3 fatty-acid to boost your mood by consuming fatty fish such as salmon, mackerel, herring, sardines, trout, pilchards and anchovies.
- Include vitamin D into your daily routine for its anti-inflammatory properties.
- Improve sleep patterns with magnesium.
- As previously mentioned, CoQ10 may be beneficial for patients with Parkinson’s Disease due to its ability to restore mitochondrial functionality (6).
References
(1) What Is Parkinson’s? Parkinson’s Foundation Web site. http://www.parkinson.org/understanding-parkinsons/what-is-parkinsons Published July 16, 2015. Accessed August 21, 2018.
(2) NCI Drug Dictionary. National Institutes of Health Web site (n.d.) https://www.cancer.gov/publications/dictionaries/cancer-drug Accessed August 21, 2018.
(3) Glutathione. Pubchem Web site. https://pubchem.ncbi.nlm.nih.gov/compound/124886 (n.d.). Retrieved Accessed August 21, 2018.
(4) Mischley, LK, Conley KE, Shankland EG, Kavanagh TJ, Rosenfeld ME, Duda JE, Padowski JM. Central nervous system uptake of intranasal glutathione in Parkinson’s disease. NPJ Parkinson’s Disease. 2016; 2:16002.
(5) Liddell JR, White, AR. Nexus between mitochondrial function, iron, copper and glutathione in Parkinson’s disease. Neurochemistry International. 2018; 117: 126–138.
(6) Encyclopedia of Natural and Alternative Treatments. ConsumerLab.com Web site. https://www.consumerlab.com/tnp.asp?chunkiid=108306#ref32 Accessed August 21, 2018.
(7) Holmay MJ, Terpstra M, Coles LD, et al. N-acetylcysteine Boosts Brain and Blood Glutathione in Gaucher and Parkinson Diseases: Clinical Neuropharmacology. 2013; 36(4):103-106.
(8) Action plan for Parkinson’s disease. Food for the Brain Web site. (n.d.). http://www.foodforthe brain.org/nutrition-solutions/parkinsons-disease/action-plan-for-parkinsons-disease.aspx Accessed August 21, 2018.
Written by Nicole Lindel, MS in Nutrition Education from Columbia University